National Sickle Cell Awareness Month was developed to raise awareness about this inherited disorder that alters red blood cells, ultimately leading to a range of serious health complications. For women, sickle cell and pregnancy, is deemed high risk. But there is hope. Under the care of maternal-fetal medicine (MFM) specialists, many women are able to carry a child to term even with a sickle cell diagnosis. And through technology advances, genetic testing can help determine when babies are at risk for the disease themselves.
The anatomy of the illness 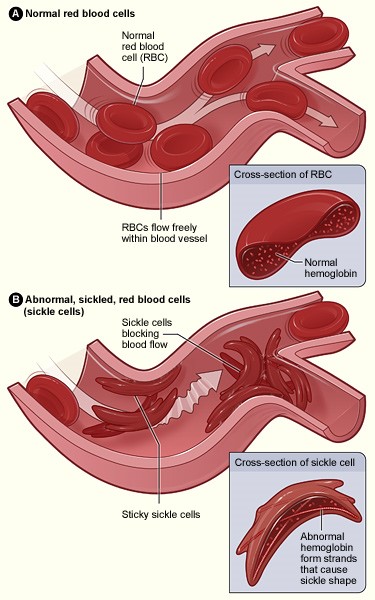
The purpose of red blood cells is to transport oxygen through our bodies, and typically, the soft rounded shape of the cells slide easily through even small blood vessels. The name “sickle” cell describes the altered shape of red blood cells in a patient. Individuals with sickle cell disease produce red blood cells that are long, rough and shaped like a crescent moon (similar to the blade of a farm tool called a sickle). The shape and texture of sickle cells can cause cells to stick together and block the flow of cells, making it harder to carry oxygen.
These blockages often lead to pain, which may become bad enough to require hospitalization. Patients with sickle cell disease universally suffer from anemia caused by their cells dying. This can result in kidney failure, heart failure, stroke and blindness. Patients may have a harder time fighting infections and experience complications with their spleens because the blood supply is more difficult to filter. Blood transfusions are a common treatment. Mothers who are carriers for sickle cell disease — meaning, they carry the sickle cell trait — do not generally have symptoms of the disease, but may be at risk if they carry another disorder such as Hemoglobin C trait or thalassemia.
(Diagram provided by National Heart, Lung, and Blood Institute)
Planning for pregnancy
During pregnancy with sickle cell disease, the intense pain and bodily damage worsens, and the risk for infections and organ issues increases. A woman could face miscarriage or preterm labor, and her baby may be born with low birth weight. Some of this is due to the fetus not receiving necessary levels of oxygen and nutrition because the mother’s red blood cells are unable to travel with ease.
For patients who have sickle cell disease, experts suggest genetic counseling before conceiving a child to ensure the parents are aware of the risks of having a child born with sickle cell disease. Preconception counseling with an MFM specialist is also recommended so that parents understand what to expect during pregnancy, including complications.
“As with most medical conditions, the best time to optimize your chance of having an uncomplicated pregnancy is before ever getting pregnant,” said Amber Samuel, MD, Medical Director of Obstetrix Medical Group of Houston. “We meet with patients to go over their risks, stop any medications that are dangerous during pregnancy and provide screening for risks to a potential baby.”
Once a woman with sickle cell disease becomes pregnant, her medical team will help explain the ways her body is reacting differently than other pregnancies — such as how and when to take supplements — and ways to protect her developing baby — such as which pain medications to avoid. Her physicians will also make her aware of the possible need for transfusion and other delivery preparations, as well as bleeding issues after the birth.
How it’s inherited
According to the World Health Organization, sickle cell disease affects millions globally. Two abnormal copies of the sickle cell gene lead to a sickle cell diagnosis. A child will inherit sickle cell disease if both the mother and the father carry one abnormal copy, or the sickle cell trait. If only one parent is affected with the disease, the baby will inherit the sickle cell trait, meaning the baby will show no signs of the illness, but will carry the gene to pass on. If only one parent is a carrier of sickle cell trait, then there is a 50 percent chance the child will be a carrier, but no risk that the child will have the disease. If both parents carry the trait, the child may be born healthy, may inherit the trait only or may inherit the full disease. Individuals of African descent are at the highest risk for developing this illness.
Our services
With 31 affiliated maternal-fetal medicine practices across the country, Obstetrix Medical Group, a MEDNAX company, provides specialized care for women with high-risk pregnancies. Our health care teams partner with local obstetricians and other specialists in the communities we serve to treat patients. Some practices also offer genetic testing services.
Reviewed by Dr. Amber Samuel
Amber Samuel, MD, completed her medical degree at Baylor College of Medicine, her obstetrics and gynecology residency at Magee-Womens Hospital of UPMC Health System and her maternal-fetal medicine fellowship at New York Presbyterian Hospital / Columbia University Medical Center. She is board certified in obstetrics and gynecology and maternal-fetal medicine. Learn more about Dr. Samuel.

